As a reminder, the horrors of severe lichen sclerosus can include all of the following and more:
- phimosis of the clitoral hood with decreased sensation and anorgasmia
- decreased blood flow,
- fissures (pain),
- itching to the point of torment
- bleeding & pain with walking,
- pain, bleeding, & tearing with defecation,
- pain with urination,
- pain and bleeding from wearing jeans (any tight clothing),
- pain, bleeding, and tearing of tissue with sex (dyspareunia), often causing years of being unable to tolerate any penetration even if aroused,
- secondary loss of libido when sex becomes associated with pain,
- permanent destruction of the labia (especially in prepubescent girls),
- all of the above torments can lead to loneliness from broken and strained love relations,
- which can lead to broken families,
- depression,
- loss of self-esteem,
- an overall painful day-to-day life.
In other words, imagine trying to enjoy just about anything while your genitalia is hurting, cracking, itching, and bleeding.
Here’s a photo of what many women who suffer from LS wake to find between their legs in the morning (often) without hope of relief after years of the usual daily clobetasol.

They also can look forward to a ten percent chance of squamous cell carcinoma with the resultant needed vulvectomy.
Lichen sclerosus is thought to be caused by the autoimmune process, hence the usual treatment—a strong topical steroid cream, clobetasol.
Unfortunately, even with clobetasol, many women continue to suffer both the tormenting symptoms and the 10% risk of squamous cell carcinoma. We need a better way.
Since the O-Shot® procedure utilizes PRP, to understand how the procedure may help those suffering from lichen sclerosus, consider all of the following:
- The effects of PRP on the autoimmune process,
- The effects of PRP on scaring,
- The effects of PRP on wound healing,
- How the O-Shot® procedure may be modified to best treat lichen sclerosus.
PRP Down-Regulates the Autoimmune Response
In thinking about the use of PRP for use in lichen sclerosus, consider other autoimmune conditions in which PRP has been shown to down-regulate the disease process.
Vitiligo treatment usually involves steroids or melanocyte transplantation, both of which can lead to unsatisfactory results. But, studies showed a dramatic improvement with PRP.
Also, alopecia areata (usually treated with steroids) responded better to PRP than to steroids in more than one study, with more and darker hair follicles when using PRP compared with steroids.
For rheumatoid arthritis (also an autoimmune process), studies demonstrated that PRP did all the following:
alleviated arthritis, and reduced humoral and cellular immune responses, leading to beneficial effects on histological parameters as observed using joint tissue histological staining. CIA mice treated with PRP exhibited downregulated expression of IL-6, IL-8, IL-17A, IL-1β, TNF-α, receptor activator for nuclear factor-κB and IFN-γ in inflammatory tissue. In addition, VEGF, PDGF, IGF‑1 and TGF-β expression in peripheral whole blood was increased following treatment with PRP. The serum concentration of anti-collagen antibody was decreased in PRP-treated CIA mice. In conclusion, CIA mice treated with PRP exhibited beneficial effects, including decreased joint inflammation, cartilage destruction and bone damage, and increased repair (Tong2017).
Even experimental autoimmune encephalitis and Bell’s Palsy (both autoimmune in etiology) have shown benefit from PRP.
With benefit shown in these and other autoimmune conditions, it is within reason that PRP may be of help in attenuating or arresting the autoimmune activity and the resultant progression of signs and symptoms of lichen sclerosus.
PRP Remodels Scar Tissue into Healthier Tissue
With the recurrent cracking, bleeding, and sclerotic changes that plague women with lichen sclerosus (LS), even if the LS is magically turned off, there is still a need to remodel the scarring from the previous activity of the disease.
PRP has been used to treat acne scars, postpartum striae, cleft-palate-repair scars, and even the scars left from devices used to treat breast cancer patients.
With the breast cancer patients, there was even seen an increased survival rate in the women who received the PRP; the authors considered it coincidental even though the benefit was statistical (Eichler2022). It’s too early to claim from this one study that PRP can protect against recurrence of breast cancer; but, similar data was seen with fat transfer for reconstruction after breast cancer. Two studies showed those who received fat (usually mixed with PRP to improve survival of the fat) showed a trend toward prolonged survival; in these two studies, the increased survival was measured but not statistically relevant. Still, these and other studies indicate that PRP is, at worst, safe in the face of women at high risk for recurrence of their breast cancer.
Apply for Online Training for the O-Shot® Procedure<--
This discussion regarding the lack of increased risk of neoplasia when using PRP is significant considering that ten percent of women with lichen sclerosus will develop squamous cell carcinoma as part of the progression and ongoing disease activity of the lichen sclerosus. One might postulate that with decreased disease activity that results from the use of PRP in some women, the risk of squamous cell carcinoma might also be decreased.
Even in women who use clobetasol like a religion, women still face a 10% risk of squamous cell carcinoma, and little is known about the effects of chronic use of clobetasol on the recurrence or occurrence of other problems like HPV (since chronic steroids could affect the local immune system). But, the fear that PRP its self may propagate neoplasia should be addressed and has been; as of yet, thousands of studies have indicated that neoplasia is not a risk when PRP is used. A growing number of studies indicate (but do not conclusively prove) that PRP may decrease the risk of neoplasia; long-term follow-up in those with lichen sclerosus needs to be done before we can claim a decreased rate of progression to squamous cell carcinoma in women who use PRP for treatment.
PRP Promotes Wound Healing
Just pretend for a moment that you have a magic wand and that if you wave that wand over the diseased tissue of a woman suffering from lichen sclerosus, then her disease activity will immediately go quiescent. Now consider this: what if your needle becomes like a magic wand for many women when you fill it with PRP? Now, you wave your magic wand, and the autoimmune process of the lichen sclerosus shuts off.
Does the woman immediately feel immediately well if you instantly turn off the disease activity?
Not at all, because she would still be left with the ravages of the process; before feeling well, she would need to replace sclerotic tissue with healthy tissue, to heal fissures, and to regrow blood vessels into the damaged tissue.
So, in effect, she would need to heal the wounds of the lichen sclerosus before she would enjoy a healthy vulva, even if you magically and instantly shut off the lichen sclerosus. Unfortunately, cortisone (used by most women to treat lichen sclerosus) delays wound healing. In comparison, a material (PRP) that both shuts off the overactive autoimmune process (and therefore shuts off the lichen sclerosus) and also promotes (rather than delaying) the healing of the damaged tissue could provide a remarkable synergy of benefits.
As we have discussed in previous sections of this report, the primary work that led to the widespread use of PRP and to the development of the devices used for the preparation of PRP began in the effort to heal surgical wounds in avascular areas like the cartilage of the knee and the bone in oral surgery. This idea of healing avascular surgical wounds with PRP extended with the publishing of many papers regarding the use of PRP to promote the healing of hard-to-heal wounds in the distal extremities of those suffering from diabetes.
Before using PRP in the genitals, I developed a method of using PRP in the face, the Vampire Facelift® for cosmetic purposes and many papers were published regarding using PRP in the scalp for reviving hair follicles. With cosmetic procedures and with hair regrowth, we are not healing a wound; instead, we are starting the cascade with PRP that would occur if there were a wound, with the result that healthier and younger-appearing tissue develops.
With lichen sclerosus, we not only face an active autoimmune process that creates sclerosis and blood vessel destruction, we also face the secondary wounds of fissures and excoriations. So, using PRP to help heal these wounds could be of great benefit.
PRP Helps Some Women with Lichen Sclerosus (both with and without phimosis)
When I first met Dr. Andrew Goldstein, he was lecturing to the International Society for Women’s Sexual Health regarding a genetic marker that could predict which women might suffer dyspareunia as a complication of taking birth control pills (yes, this is a known complication). He also revealed to the audience that he was in the process of passing a kidney stone while he was giving the lecture! I found his lecture to be brilliant and his grit to be impressive.
So, after his talk, I approached him about the possibility of doing research together. Knowing of my work with the O-Shot® procedure, he suggested we do a study regarding the use of PRP for lichen sclerosus. At that time, Dr. Casabona had published an article demonstrating that stem cells would improve lichen sclerosus but no one had published anything regarding PRP for LS.
I agreed to sponsor the study on the spot, and we exchanged numbers.
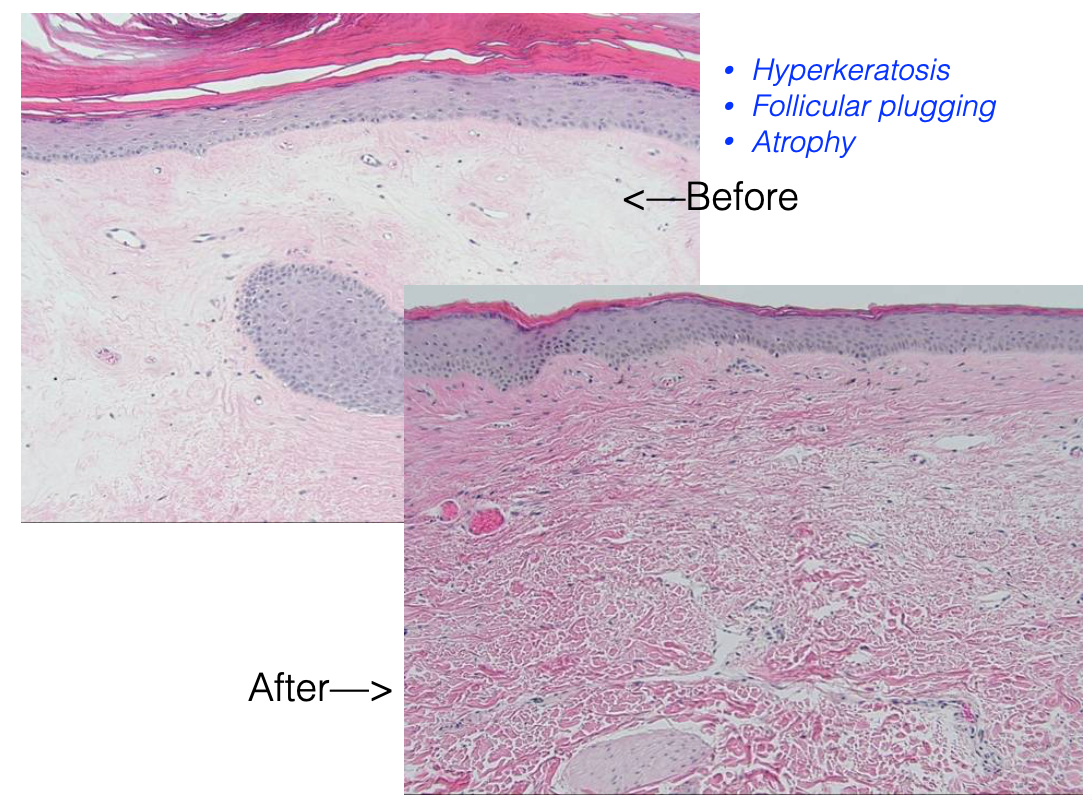
Some months later, we published a study where women suffering from LS were biopsied, treated with PRP, and then surveyed for changes in symptoms and re-biopsied. Two dermatopathologists with much experience with LS were blinded to which was the before and which was the after biopsy. Both the surveys of the women and the biopsies demonstrated a statistical improvement in lichen sclerosus after treatment with PRP. We then extended the numbers of women in the study and published a second paper—also showing a statistical benefit to PRP for LS. These were the first two studies to show the benefit of LS after treatment with PRP using a variation of our O-Shot® procedure.
Then, after our second study, a woman who suffered with lichen sclerosus and who had been greatly helped by PRP, sponsored a third study. In this study (done without my participation), saline was used as a placebo. In other words , the women in one group were injected with PRP and the women in the second group were injected with saline.
Ironically, in this third study (sponsored by a woman who’s LS improved after treatment with PRP), where saline was used as a placebo, there was no statistical difference between the placebo group and the PRP group; but, 50% of the women in the placebo group improved!
In short, both groups got better, and the group that was injected with PRP did better than the saline group; but because there was such a strong response rate in the “placebo” group, there was not a statistical difference between the two and the authors concluded that PRP does not work.
Put another way: a generous woman suffering from LS who got better with PRP paid for a study of treating LS with PRP—and the authors she hired concluded that there was “no benefit” from PRP, the same treatment that got the woman financier well.
I think something more important was shown by the study than that PRP does not help LS: the research further demonstrates the idea shown by others that saline, when used for hydrodissection, is not a placebo. Saline can even be used to treat scars and even to decrease pain.
Especially when saline is injected in such a way that it causes hydrodissection, there can be measurable changes in the tissue resulting from the resultant micro-trauma followed by post-op healing.
So, in this third study, Dr. Goldstein and his collaborators concluded (in contradiction to our previous two studies) that PRP offers no benefit. But, this was a study with biopsies, not simply a survey; I cannot find another study of LS where 50% of the placebo group improved on biopsy. I think that Dr. Goldstein showed something more important than what he reported; I think his study showed that hydrodissection alone precipitates changes (as has been shown with other conditions) that improve LS and that PRP can be used for the hydrodissection for benefits measurably better than saline alone.
In other words, I think what Dr. Goldstein showed was that, with our O-Shot®, there is not simply a biological effect from the growth factors; there is also a mechanical effect—essentially a surgical effect—from the mechanical hydrodissection of injecting the PRP.
I have tremendous respect for Dr. Goldstein and his knowledge of lichen sclerosus, but I think my interpretation of his research can be different than his and still maintain great respect for his work.
Put simply; the O-Shot® is a mechanical procedure combined with a biochemical cascade.
Other studies have since been published showing that PRP can improve lichen sclerosus.
The O-Shot® for Those with Phimosis
A woman of fifty-three years old came to my office because she had been unable to tolerate her husband’s penis for 7 years because of her lichen sclerosus. She was using daily clobetasol and being followed by her dermatologist with regular visits for the entire 7 years.
In addition to being unable to tolerate more than about two inches of one of my fingers inserted into her vagina because her clitoris was completely covered by her phimosed clitoral hood, she reported that she enjoyed very little pleasure from her attempts to masturbate.
Her husband, who came with her to my office, as is often the case, seemed loving and content but suffered empathetically for his wife because she enjoyed very little sexual pleasure of any kind. There is this idea in some circles that women only want to heal their vagina so they can please their husbands and that we should just leave such women alone, that if it were not for demanding men that they would be just fine; but, if you see only a few women with LS, you realize how very wrong is that idea; husband or no husband, women with LS can lose the ability to enjoy sexual pleasure and often feel broken and alone.
In the following photograph, the first image on the far left shows her vagina on the day she came to my office.

I injected her labia, clitoral hood, the clitoris (through the hood), the entire area, and the anterior vagina wall.
I am not a surgeon, so I sent her to an excellent board-certified gynecologist near my office, Dr. Kathleen Posey, who then dissected out the clitoris—freeing it from the scaring phimosis that had it trapped.
Research has shown that with LS even if the hood is completely phimosed such that the clitoris is unreachable, the clitoris is not directly affected by LS and, when freed, will function normally.
Dr. Posey took the second photo (the one in the middle) on the day she freed the clitoris.

Normally, with such a surgery in a woman suffering from LS, there would likely be a quick recurrence of sclerosis with re-entrapment of the clitoris beneath the LS-diseased clitoral hood.
Instead of the hood re-phimosing, six weeks later, Dr. Posey took the photograph on the far right demonstrating that the hood and labia had grown healthier in appearance, and the woman reported she was having comfortable sex with her husband for the first time in over seven years—off of her clobetasol!

She continues to get a modified O-Shot® from Dr. Posey every year or so and to enjoy comfortable sex.
Dr. Posey went on to treat other women in this way and published her findings (Posey2015).
Next Hands-On Workshops<--
Alexandra Runnels, MD, sent photos of a patient who had ten years of Clobetasol and was working as a soldier—imagine marching, and that’s what you have to remind yourself with itching, burning, and bleeding—every time you take a step with your pack.
And then, after stopping the Clobetasol—she achieved the results on the right by using a combination of PRP with micro-needling to the more sclerotic areas and the usual 2-injection O-Shot®, combined with injecting PRP into the area and using daily UVB light, combined with Altar® cream to achieve the much healthier tissue (see below).

The phimosis surgery was done about 8 weeks after the first PRP treatment. Her marriage and her self-image and her life changed for the better.
O-Shot® Variations for the Treatment of Lichen Sclerosus
- Techniques: For phimosis, after you dissect the clitoris to freedom, then injecting with PRP and micro-needling the more sclerotic areas seems to work well in about 80% of women with LS.
-
This summary neither qualifies nor fully instructs in the O-Shot® procedure for lichen sclerosus. Application for training can be found here<-- or by callling the Cellular Medicine Association at 1-888-920-5311
- Not all women respond; if no improvement, they go back on clobetasol.
- Stop clobetasol 3-5 days before the treatment and see the woman back in 3 to 6 weeks.
- Reinject on sec0nd visit any active areas.
- Expect to need to reinject every six to eighteen months.
- Works in synergy with UV light
- Have a low threshold for rebiopsy.
- Bring back at least once every 6 months to revaluate.
Find the nearest provider of the O-Shot® procedure for licen sclerosus<--
Summary
- PRP, when injected in some women suffering from lichen sclerosus, provides a dramatic down-regulation of their disease.
- There is, of yet, no sure-fire “cure” for lichen sclerosus. Not everyone responds to PRP and those who do usually require repeated treatments every nine to eighteen months. Also, not everyone finds complete relief from clobetasol. It does appear that some who do not find relief from clobetasol do find relief from PRP and vice versa.
- Those who do not respond to PRP should be put back on clobetasol. Those who find complete relief from clobetasol may not need PRP.
- Biopsies should always be done regularly as we do not yet have a sure way of preventing the progression of lichen sclerosus to squamous cell carcinoma—clobetosol does not completely prevent the progression and it’s unlikely that PRP completely prevents the progression.
- Studies of other diseases processes (like breast cancer), and over 15,000 published papers on PubMed regarding PRP without complication from neoplasia, indicate that PRP does not increase the risk of neoplasia.
- If PRP is carcinogenic, then every surgery should be carcinogenic, considering the same growth factors are released from platelets in the healing of a surgical wound as are released from PRP.
- It seems logical that in the women who respond to the O-Shot® procedure, there would be less risk of squamous cell carcinoma since the disease seems to go quiescent, but we do not yet know if this is the case.
References
Research Regarding the Use of PRP for Autoimmune Disease
- Vazquez OA, Safeek RH, Komberg J, Becker H. Alopecia Areata Treated with Advanced Platelet-rich Fibrin Using Micronization. Plast Reconstr Surg Glob Open. 2022;10(1):e4032. doi:10.1097/GOX.0000000000004032
- Anitua E, Pino A, Aspe L, et al. Anti-inflammatory effect of different PRGF formulations on cutaneous surface. Journal of Tissue Viability. 2021;30(2):183-189. doi:10.1016/j.jtv.2021.02.011
- Huber SC, de Lima Montalvão SA, Sachetto Z, Santos Duarte Lana JF, Annichino-Bizzacchi JM. Characterization of autologous platelet rich plasma (PRP) and its biological effects in patients with Behçet’s Disease. Regen Ther. 2021;18:339-346. doi:10.1016/j.reth.2021.08.010
- Rekik M, Mseddi M, Nadine K, Sellami K, Turki H. Efficacy of autologous platelet-rich plasma in the treatment of vitiligo : A 10- patient prospective study. Journal of Cosmetic Dermatology. n/a(n/a). doi:10.1111/jocd.15050
- Tong S, Zhang C, Liu J. Platelet-rich plasma exhibits beneficial effects for rheumatoid arthritis mice by suppressing inflammatory factors. Mol Med Rep. 2017;16(4):4082-4088. doi:10.3892/mmr.2017.7091
- Seffer I, Nemeth Z. Recovery from Bell Palsy after Transplantation of Peripheral Blood Mononuclear Cells and Platelet-Rich Plasma: Plastic and Reconstructive Surgery – Global Open. 2017;5(6):e1376. doi:10.1097/GOX.0000000000001376
- Pototschnig H, Madl MT. Successful Treatment of Alopecia Areata Barbae with Platelet-rich Plasma. Cureus. 2020;12(4):e7495. doi:10.7759/cureus.7495
- Trink A, Sorbellini E, Bezzola P, et al. A randomized, double-blind, placebo- and active-controlled, half-head study to evaluate the effects of platelet-rich plasma on alopecia areata. British Journal of Dermatology. 2013;169(3):690-694. doi:10.1111/bjd.12397
- Borhani-Haghighi M, Mohamadi Y. The therapeutic effect of platelet-rich plasma on the experimental autoimmune encephalomyelitis mice. J Neuroimmunol. 2019;333:476958. doi:10.1016/j.jneuroim.2019.04.018
- Behnia-Willison F, Pour NR, Mohamadi B, et al. Use of Platelet-rich Plasma for Vulvovaginal Autoimmune Conditions Like Lichen Sclerosus. Plast Reconstr Surg Glob Open. 2016;4(11):e1124. doi:10.1097/GOX.0000000000001124
-
Pensato R, La Padula S. The Effect of Lipofilling and Platelet-Rich Plasma on Patients with Moderate–Severe Vulvar Lichen Sclerosus Who were Non-responders to Topical Clobetasol Propionate: A Randomized Pilot Study. Aesth Plast Surg. Published online May 31, 2022. doi:10.1007/s00266-022-02947-y
Research Showing PRP Remodels Scar Tissue
- Alves R, Grimalt R. A Review of Platelet-Rich Plasma: History, Biology, Mechanism of Action, and Classification. Skin Appendage Disord. 2018;4(1):18-24. doi:10.1159/000477353
- Gawdat H, El-Hadidy YA, Allam RSHM, Abdelkader HA. Autologous platelet-rich plasma “fluid” versus “gel” form in combination with fractional CO2 laser in the treatment of atrophic acne scars: a split-face randomized clinical trial. Journal of Dermatological Treatment. 2022;0(ja):1-31. doi:10.1080/09546634.2022.2067816
- Charles-de-Sá L, Gontijo-de-Amorim NF, Takiya CM, et al. Effect of Use of Platelet-Rich Plasma (PRP) in Skin with Intrinsic Aging Process. Aesthet Surg J. 2018;38(3):321-328. doi:10.1093/asj/sjx137
- Eichler C, Üner J, Thangarajah F, et al. Platelet-rich plasma (PRP) in oncological patients: long-term oncological outcome analysis of the treatment of subcutaneous venous access device scars in 89 breast cancer patients. Arch Gynecol Obstet. Published online April 4, 2022. doi:10.1007/s00404-022-06416-4
- Number 5 SV 24. Platelet-Rich Plasma (PRP): Current Applications in Dermatology. Accessed August 26, 2021. https://www.skintherapyletter.com/dermatology/platelet-rich-plasma-prp/
- Sánchez M, Anitua E, Delgado D, et al. Platelet-rich plasma, a source of autologous growth factors and biomimetic scaffold for peripheral nerve regeneration. Expert Opinion on Biological Therapy. 2017;17(2):197-212. doi:10.1080/14712598.2017.1259409
Research Showing the PRP Promotes Wound Healing
- Autologous platelet-rich plasma vs conventional dressing in the management of chronic diabetic foot ulcers – PubMed. Accessed March 7, 2022. https://pubmed.ncbi.nlm.nih.gov/35108667/
- Pourkarim R, Farahpour MR, Rezaei SA. Comparison effects of platelet-rich plasma on healing of infected and non-infected excision wounds by the modulation of the expression of inflammatory mediators: experimental research. Eur J Trauma Emerg Surg. Published online February 12, 2022. doi:10.1007/s00068-022-01907-0
- García-Sánchez JM, Mirabet Lis V, Ruiz-Valls A, Pérez-Plaza A, Sepúlveda Sanchis P, Pérez-del-Caz MD. Platelet rich plasma and plasma rich in growth factors for split-thickness skin graft donor site treatment in the burn patient setting: A randomized clinical trial. Burns. Published online October 22, 2021. doi:10.1016/j.burns.2021.10.001
- Chicharro-Alcántara D, Rubio-Zaragoza M, Damiá-Giménez E, et al. Platelet Rich Plasma: New Insights for Cutaneous Wound Healing Management. J Funct Biomater. 2018;9(1):10. doi:10.3390/jfb9010010
- Spanò R, Muraglia A, Todeschi MR, et al. Platelet-rich plasma-based bioactive membrane as a new advanced wound care tool. Journal of Tissue Engineering and Regenerative Medicine. 2018;12(1):e82-e96. doi:10.1002/term.2357
- Saputro ID, Rizaliyana S, Noverta DA. The effect of allogenic freeze-dried platelet-rich plasma in increasing the number of fibroblasts and neovascularization in wound healing. Ann Med Surg (Lond). 2022;73:103217. doi:10.1016/j.amsu.2021.103217
- Kelm RC, Ibrahim O. Utility of platelet-rich plasma in aesthetics. Clinics in Dermatology. 2022;40(1):19-28. doi:10.1016/j.clindermatol.2021.08.007
Research Regarding Fat Transfer to the Breast and No Increased Risk of Breast Cancer and that PRP is Safe with a History of Breast Cancer
Research Showing Improvement of Lichen Sclerosus with UVB
Research Regarding Steroids Reactivating Papilloma Virus
von Krogh G, Dahlman-Ghozlan K, Syrjänen S. Potential human papillomavirus reactivation following topical corticosteroid therapy of genital lichen sclerosus and erosive lichen planus. Journal of the European Academy of Dermatology and Venereology : JEADV. 2002;16(2):130-133. Accessed August 24, 2015. http://www.ncbi.nlm.nih.gov/pubmed/12046814
Research Showing that PRP Helps Women Suffering from Lichen Sclerosus
- Goldstein AT, Mitchell L, Govind V, Heller D. A Randomized Double-Blind Placebo Controlled Trial of Autologous Platelet Rich Plasma Intradermal Injections for the Treatment of Vulvar Lichen Sclerosus. Journal of the American Academy of Dermatology. Published online January 2019. doi:10.1016/j.jaad.2018.12.060
- Msc MK, Tolson H, Runels C, Gloth M, Pfau R, Goldstein AT. Autologous Platelet Rich Plasma (PRP) Intradermal Injections for the Treatment of Vulvar Lichen Sclerosus. Journal of Lower Genital Tract Disease. 2015;19(3):S1-S25. http://journals.lww.com/jlgtd/Fulltext/2015/07001/ISSVD2015Abstracts.2.aspx
- Casabona F, Gambelli I, Casabona F, Santi P, Santori G, Baldelli I. Autologous platelet-rich plasma (PRP) in chronic penile lichen sclerosus: the impact on tissue repair and patient quality of life. Int Urol Nephrol. 2017;49(4):573-580. doi:10.1007/s11255-017-1523-0
- Mitchell L, Goldstein AT, Heller D, et al. Fractionated Carbon Dioxide Laser for the Treatment of Vulvar Lichen Sclerosus: A Randomized Controlled Trial. Obstetrics & Gynecology. 2021;137(6):979-987. doi:10.1097/AOG.0000000000004409
- Goldstein AT, King M, Runels C, Gloth M, Pfau R. Intradermal injection of autologous platelet-rich plasma for the treatment of vulvar lichen sclerosus. Journal of the American Academy of Dermatology. 2017;76(1):158-160. doi:10.1016/j.jaad.2016.07.037
- Posey K, Runels C. In-Office Surgery and Use of Platelet Rich Plasma for Treatment of Vulvar Lichen Sclerosus to Alleviate Painful Sexual Intercourse. Journal of Lower Genital Tract Disease. 2015;19(3):S1-S25. doi:10.1097/lgt.0000000000000121
- ISSVD 2015 Abstracts. Journal of Lower Genital Tract Disease. 2015;19(3):S1-S25. doi:10.1097/lgt.0000000000000121
- Lee A, Bradford J, Fischer G. Long-term management of adult vulvar lichen sclerosus: a prospective cohort study of 507 women. JAMA Dermatol. 2015;151:1061-1067.
- Casabona F, Priano V, Vallerino V, Cogliandro A, Lavagnino G. New surgical approach to lichen sclerosus of the vulva: the role of adipose-derived mesenchymal cells and platelet-rich plasma in tissue regeneration. Plastic and reconstructive surgery. 2010;126(4):210e-211e.
- Franic D, Iternička Z, Franić-Ivanišević M. Platelet-rich plasma (PRP) for the treatment of vulvar lichen sclerosus in a premenopausal woman: A case report. Case reports in women’s health. 2018;18:e00062. doi:10.1016/j.crwh.2018.e00062
- Smith JG. The journal of the American Academy of Dermatology. International journal of dermatology. 2005;18(6):466-467. http://www.ncbi.nlm.nih.gov/pubmed/19539853
- Vittrup G, Mørup L, Heilesen T, Jensen D, Westmark S, Melgaard D. The Quality of Life and Sexuality in Women with Lichen Sclerosus – A Cross Sectional Study. Clinical and Experimental Dermatology. n/a(n/a). doi:10.1111/ced.14893
- Tedesco M, Pranteda G, Chichierchia G, al. et. The use of PRP (platelet-rich plasma) in patients affected by genital lichen sclerosus: clinical analysis and results. J Eur Acad Dermatol Venereol. 2019;33:e58-e59.
- Marnach ML, Torgerson RR. Therapeutic Interventions for Challenging Cases of Vulvar Lichen Sclerosus and Lichen Planus. Obstetrics & Gynecology. 2021;138(3):374-378. doi:10.1097/AOG.0000000000004498
- Behnia-Willison F, Pour NR, Mohamadi B, et al. Use of Platelet-rich Plasma for Vulvovaginal Autoimmune Conditions Like Lichen Sclerosus: Plastic and Reconstructive Surgery – Global Open. 2016;4(11):e1124. doi:10.1097/GOX.0000000000001124
- Corazza M, Schettini N, Zedde P, Borghi A. Vulvar Lichen Sclerosus from Pathophysiology to Therapeutic Approaches: Evidence and Prospects. Biomedicines. 2021;9(8):950. doi:10.3390/biomedicines9080950
- Krapf JM, Mitchell L, Holton MA, Goldstein AT. Vulvar Lichen Sclerosus: Current Perspectives. IJWH. 2020;Volume 12:11-20. doi:10.2147/IJWH.S191200
Research Indicating the Saline Is Not Be A Placebo When Used for Hydrodissection
- Clinical benefit of intra-articular saline as a comparator in clinical trials of knee osteoarthritis treatments A systematic review and meta-analysis of randomized trials | Elsevier Enhanced Reader. doi:10.1016/j.semarthrit.2016.04.003
- Sharma R, Gupta M, Rani R. Delineating injectable triamcinolone-induced cutaneous atrophy and therapeutic options in 24 patients—A retrospective study. Indian Dermatol Online J. 2022;13(2):199. doi:10.4103/idoj.idoj48321
- Asghar A, Tahir Z, Ghias A, Iftikhar U, Ahmad TJ. Efficacy and Safety of Intralesional Normal Saline in Atrophic Acne Scars. Annals of King Edward Medical University. 2019;25(2). doi:10.21649/akemu.v25i2.2867
- Bagherani N, R Smoller B. Introduction of a novel therapeutic option for atrophic acne scars: saline injection therapy. Glob Dermatol. 2016;2(6). doi:10.15761/GOD.1000159
- Searle T, Al-Niaimi F, Ali FR. Saline in dermatologic surgery. Journal of Cosmetic Dermatology. 2021;20(4):1346-1347. doi:10.1111/jocd.13996
- El-Amawy HS, Sarsik SM. Saline in Dermatology: A literature review. Journal of Cosmetic Dermatology. 2021;20(7):2040-2051. doi:10.1111/jocd.13813
- Saltzman BM, Leroux T, Meyer MA, et al. The Therapeutic Effect of Intra-articular Normal Saline Injections for Knee Osteoarthritis: A Meta-analysis of Evidence Level 1 Studies. Am J Sports Med. 2017;45(11):2647-2653. doi:10.1177/0363546516680607



Leave a Reply