From Leaking Urethra to Damaged Prostate
Most women who undergo a mid-urethral sling (MUS) placement will see an improve sexual function, but 1 in 11 women will suffer a decrease in sexual pleasure after the procedure.
Midurethal sling: Better sex for most women; but 1 in 11 suffers more?
One in 11 suffers more.
So, to better understand the reason for this unwanted result (of decreased sexual pleasure in 1 in 11 women who undergo MUS), Guadet et al. performed mid-urethral slings on cadavers and then sectioned the area to visualize the affected tissue. They reported their results in the Journal of Sexual Medicine in 2018 as follows:
“MUS placement interrupts tissue with glandular, vascular, and neuronal structures within the periurethral space adjacent to the anterior vaginal wall. Disruption of the prostatic glandular tissue and neurovascular structures may be a root cause of orgasmic dysfunction and diminished sexual satisfaction evident in women following MUS implantation.”
Recovering Function (or Preventing Dysfunction) in Regards to MUS
Considering the previous description, to correct or prevent the problem, where would you inject a material which increases blood flow, grows nerves and collagen, improves the health of glandular tissue, and has never been reported to form a granuloma or neoplasia?
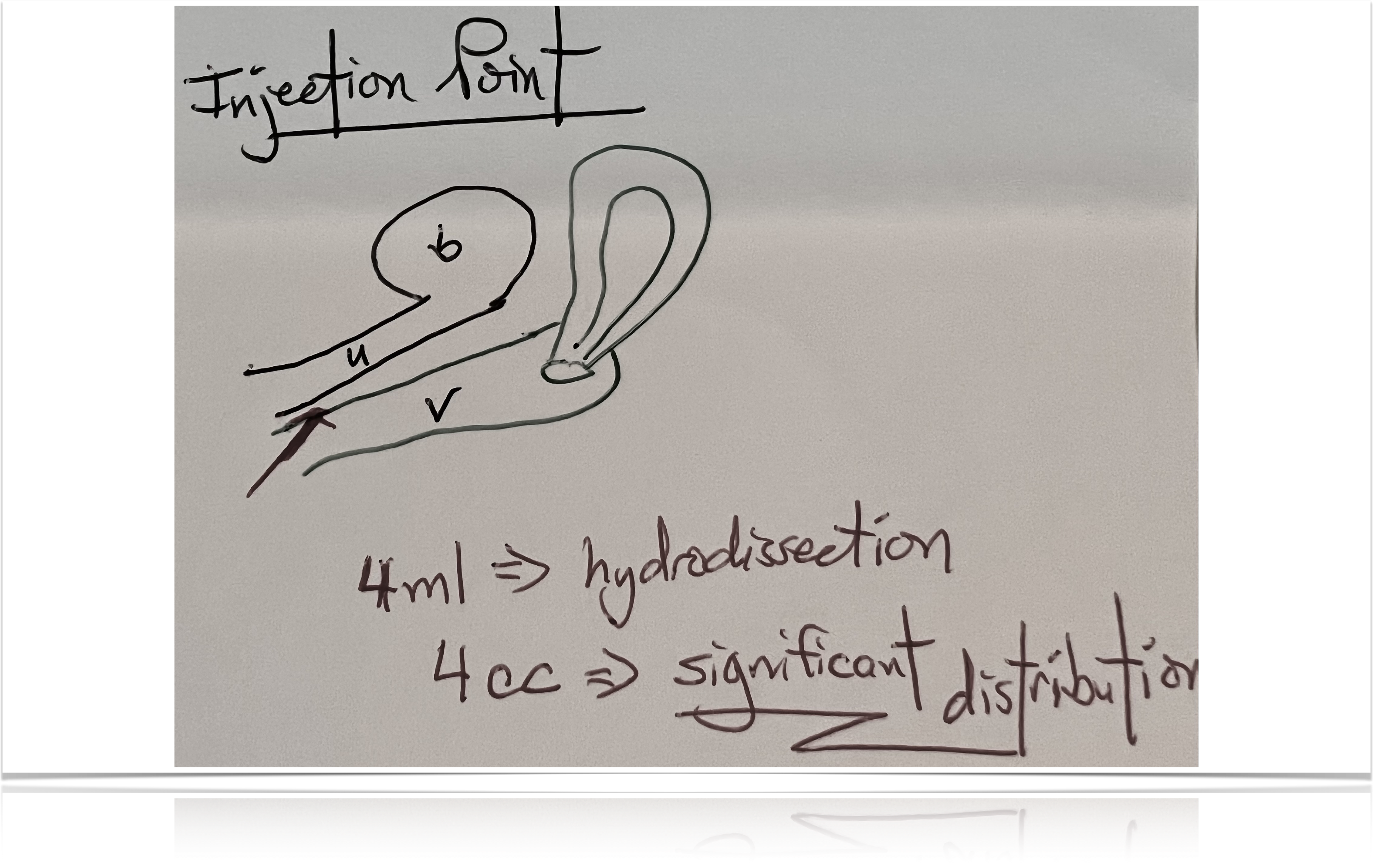
Also, consider that the material you will inject is aqueous, so it will hydrodissect along the tissue planes, taking the path of least resistance as if you were hydrodissecting with saline. This means you would not need multiple injections since you could use the pressure gradient generated by your syringe to spread the material.
Now, look at the following diagram, the same one we used to describe (in Section 1) what could be the best of the currently published options for the placement of the needle for the injection of PRP for the treatment of stress urinary incontinence (the O-Shot® procedure).
Then take another look at the photograph of the placement of the needle for the O-Shot® procedure:
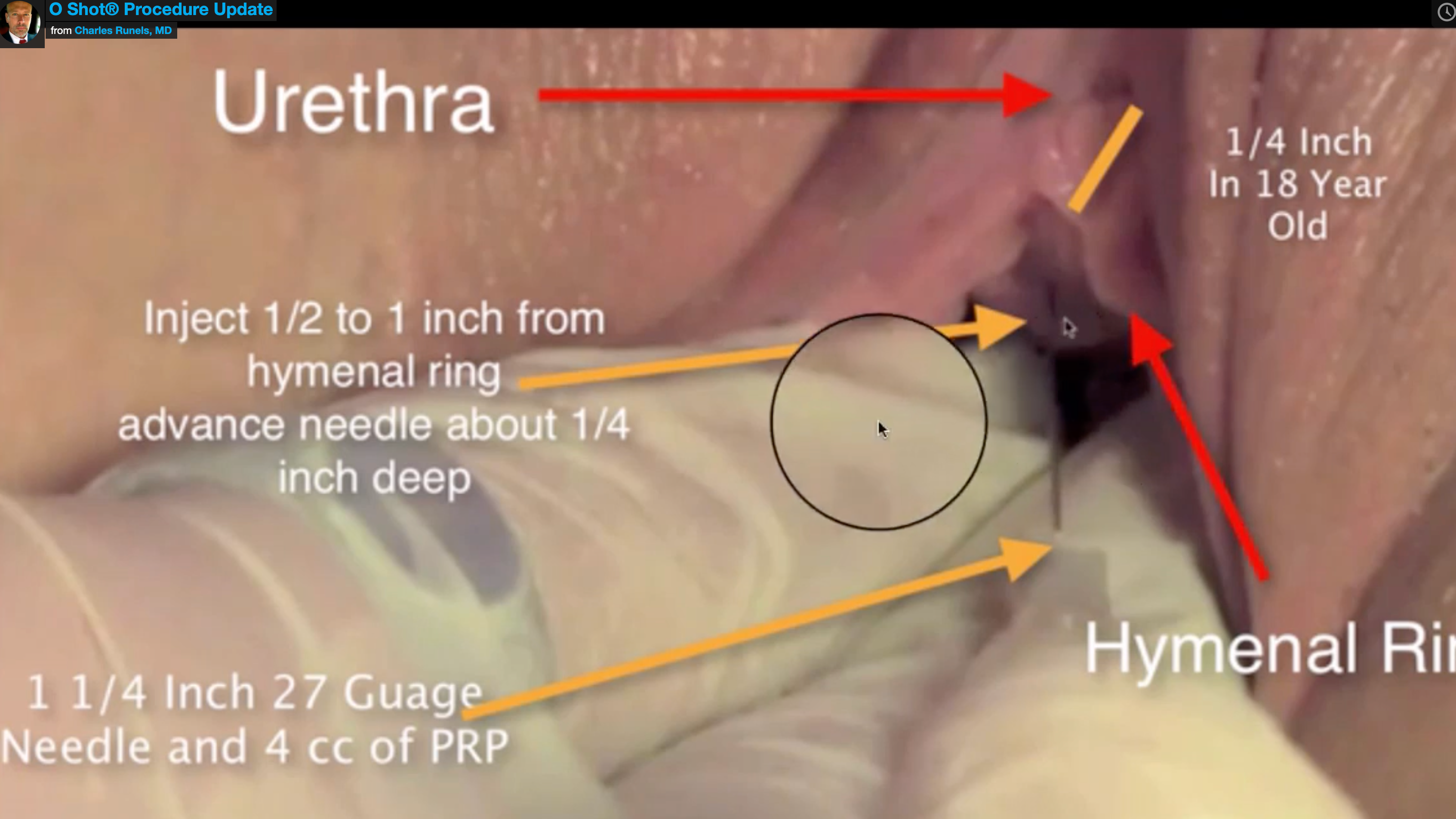
Now you can see that our O-Shot® procedure is designed to repair exactly where these brilliant investigators documented that the neurovascular damage from a MUS occurs. (Application for further training in the O-Shot® procedure can be found at OShot.info/members (click), this description does not constitute training or license to use the name “O-Shot,” which is protected by the US Patent & Trademark office for license to only those approved by the Cellular Medicine Association.
My Third Female-Ejaculation Experience, Which Leads to the O-Shot® Procedure
In 1984, while in medical school, one of our professors said to the class, “I do not want anyone to finish at this medical school and still think that female ejaculation is not a real phenomenon.”
Then, he showed us a video of a woman masturbating until she ejaculated.
Watching the video, I thought, “Looks like an interesting party trick; but of what practical benefit does that serve except the knowledge that the female body can ejaculate.”
Years later, a lover demonstrated to me that she could bring herself to masturbation with ejaculation. I still found the phenomenon interesting but not warranting much attention.
Then, it happened.
While I was making love to a woman, she unexpectedly ejaculated for the first time; and, unlike what I had witnessed with the previous two demonstrations (ejaculation while masturbating) when she ejaculated during our lovemaking, not only could I almost feel the deep, soul-shattering depth of her orgasm, but also her demeanor afterward reflected that of a man after ejaculation with calmness, satisfied bliss, and a wanting to connect with me emotionally like I had never witnessed with this woman—perhaps with any woman.
Finally, I took notice.
Up until then, the female orgasms that I had witnessed were associated with women showing varying degrees of pleasure during the orgasm, followed by increased energy and increased hunger for more sex and more orgasms. But, observing my third female ejaculation, the woman afterward showed calmness and peace and greatly decreased energy and complete satisfaction; more importantly, she seemed to drop invisible walls and swing open a wide path from her soul to mine.
I concede that my description of female ejaculation does not provide a scientific-objective explanation of what happened; but hopefully, you will forgive the description when you consider that when I find world-renowned experts in female sexuality and ask them to describe it to me in scientific-objective words, what happens when a woman experiences an orgasm of any kind, I can see their frustration as they give what we both know to be a relatively superficial answer to a profoundly important phenomenon.
So, since there is no good scientific explanation of the frequent orgasms of usual lovemaking (in comparison with a soul-shaking orgasm where the woman sobs, ejaculates and melts her soul into yours), I hope that you will pardon my use of a subjective description where no objective measure exists. Something happens to more easily facilitate a soul connection between a woman and her lover (and maybe even her GOD) when she experiences an ejaculatory orgasm.
After experiencing for the first time this phenomenon of female ejaculatory orgasm during lovemaking, I decided to pay more attention; I began reading all the popular books, the textbooks, and the research that I could find regarding female ejaculation. And, I began learning more about my lover (and subsequent lovers) about how to reproduce and enhance the experience of the female ejaculatory orgasm.
William Osler once told his medical students that if he asked them how long it takes for the fingernail to grow one length, most of them would not give it a second thought; some of them would read about it; and a few of them would grab a silver nitrate stick, make a mark on their proximal thumbnail with the stick, and then measure how long it took for the mark to grow to the end of the finger.
It was in the spirit of the third medical student described by Dr. Olser that I read the books and the research for the next ten-plus years and then took that reading to the bedroom. Over more than a decade, I developed my own ideas about female ejaculation. I even published an online course for men about how to help their female lover to a complete and profound ejaculatory orgasm and have helped thousands of couples with that course.
I tell you about my interest in female ejaculation for only one purpose: to show you that the study of female ejaculation combined with my work providing hormone replacement and menopausal care for over 3,000 women is what set the stage for me to design the O-Shot® procedure.
Then, in early 2010, I was first introduced to the idea of PRP and its possibilities for cosmetic use in the face. Because the stage was set, one of the ideas that occurred to me regarding PRP was to inject it near the distal urethra in the area of the Skene’s glands (female prostate) to see if it would enhance the female ejaculatory orgasm. During this time, I had already developed the P-Shot® and injected my own corpus cavernosi (penis) multiple times, so it seemed reasonable also to inject the female corpus cavernosi and periurethral area as well.
The best I can tell, I was the first to inject (2010) the female periurethral area with PRP.
First, I injected my lover; I had taught her to have an ejaculatory orgasm and wanted to see if things would improve. Afterward, her ejaculatory orgasms grew consistently higher on the Richter scale.
I thought maybe her results were just a placebo effect. Then, knowing that PRP has been shown in multiple studies to remodel scar tissue into a more healthy state, I injected a woman’s periurethral and clitoral area who had been physically abused by her x-husband—leaving her with severe dyspareunia and anorgasmia even after seeing multiple gynecologists.
So, she received the second O-Shot® procedure.
Afterward, not only did her dyspareunia resolve, but also she reported to me that she was able to start running again because her urinary incontinence went away.
I thought, “Why didn’t I think of that?!”
In the process of injecting in the area of the Skene’s glands (or female prostate), I had inadvertently chosen a place that would help urinary incontinence and improve the nerves associated with sexual function and micturition.
Since then, we (members of the Cellular Medicine Association) have found that injecting more proximal to the bladder does not affect the entire urethra as significantly with resultantly less improvement for both urinary incontinence and for sex.
So, my process of designing the place to put the PRP to improve ejaculatory orgasm inadvertently resulted in placing the PRP where it would best help those suffering from urinary incontinence or with sexual dysfunction after a sling.
Summary
- Most women see an improvement in sexual function after a mid-urethral sling.
- One in 11 women sees a decrease in sexual function after a sling.
- Cadaver studies showed that the nerves, Skene’s glands, and blood flow disrupted by the placement of a MUS lie exactly where the PRP is placed when doing the O-Shot® procedure.
- PRP is aqueous and therefore requires a minimum of injection points if the needle lumen is put into the proper tissue plane to affect best the tissue that needs repair.
- Meticulous placement of the PRP for improvement of sex after MUS placement is critical to the success of the procedure.
- Reading this report does not qualify anyone to do an O-Shot® procedure; many critical nuances are beyond the scope of this report.
- Application for training in the O-Shot® procedure can be found at OShot.info/members.
References
- Jang HC, Jeon JH, Kim DY. Changes in Sexual Function after the Midurethral Sling Procedure for Stress Urinary Incontinence: Long-term Follow-up. Int Neurourol J. 2010;14(3):170. doi:10.5213/inj.2010.14.3.170
- Gaudet D, Clohosey DG, Hannan JL, et al. 249 Midurethral sling placement disrupts periurethral neurovascular and glandular structures near anterior vaginal wall: Potential role in female sexual dysfunction. The Journal of Sexual Medicine. 2018;15(7):S221-S222. doi:10.1016/j.jsxm.2018.04.214
- Runels C. A Pilot Study of the Effect of Localized Injections of Autologous Platelet Rich Plasma (PRP) for the Treatment of Female Sexual Dysfunction. J Women’s Health Care. 2014;03(04). doi:10.4172/2167-0420.1000169
- Gaudet D, Clohosey DG, Hannan JL, et al. 249 Midurethral sling placement disrupts periurethral neurovascular and glandular structures near anterior vaginal wall: Potential role in female sexual dysfunction. The Journal of Sexual Medicine. 2018;15(7):S221-S222. doi:10.1016/j.jsxm.2018.04.214
- Rodriguez FD, Camacho A, Bordes SJ, Gardner B, Levin RJ, Tubbs RS. Female ejaculation: An update on anatomy, history, and controversies. Clin Anat. 2021;34(1):103-107. doi:10.1002/ca.23654
- Pollen JJ, Dreilinger A. Immunohistochemical identification of prostatic acid phosphatase and prostate specific antigen in female periurethral glands.
Urology. 1984;23(3):303-304. doi:10.1016/S0090-4295(84)90053-0 - Korda JB, Goldstein SW, Sommer F. SEXUAL MEDICINE HISTORY: The History of Female Ejaculation. The Journal of Sexual Medicine. 2010;7(5):1965-1975. doi:10.1111/j.1743-6109.2010.01720.x
- Tomalty D, Giovannetti O, Hannan J, et al. Should We Call It a Prostate? A Review of the Female Periurethral Glandular Tissue Morphology, Histochemistry, Nomenclature, and Role in Iatrogenic Sexual Dysfunction. Sexual Medicine Reviews. 2022;0(0). doi:10.1016/j.sxmr.2021.12.002
- Dietrich W, Susani M, Stifter L, Haitel A. The Human Female Prostate—Immunohistochemical Study with Prostate‐Specific Antigen, Prostate‐Specific Alkaline Phosphatase, and Androgen Receptor and 3‐D Remodeling. The Journal of Sexual Medicine. 2011;8(10):2816-2821. doi:10.1111/j.1743-6109.2011.02408.x
- Zavia M. Ultrastructure of the normal adult human female prostate gland (Skene’s gland). :12.
- Alves R, Grimalt R. A Review of Platelet-Rich Plasma: History, Biology, Mechanism of Action, and Classification. Skin Appendage Disord. 2018;4(1):18-24. doi:10.1159/000477353
- Gawdat H, El-Hadidy YA, Allam RSHM, Abdelkader HA. Autologous platelet-rich plasma “fluid” versus “gel” form in combination with fractional CO2 laser in the treatment of atrophic acne scars: a split-face randomized clinical trial. Journal of Dermatological Treatment. 2022;0(ja):1-31. doi:10.1080/09546634.2022.2067816
- Charles-de-Sá L, Gontijo-de-Amorim NF, Takiya CM, et al. Effect of Use of Platelet-Rich Plasma (PRP) in Skin with Intrinsic Aging Process. Aesthet Surg J. 2018;38(3):321-328. doi:10.1093/asj/sjx137
- Eichler C, Üner J, Thangarajah F, et al. Platelet-rich plasma (PRP) in oncological patients: long-term oncological outcome analysis of the treatment of subcutaneous venous access device scars in 89 breast cancer patients. Arch Gynecol Obstet. Published online April 4, 2022. doi:10.1007/s00404-022-06416-4
- Number 5 SV 24. Platelet-Rich Plasma (PRP): Current Applications in Dermatology. Accessed August 26, 2021. https://www.skintherapyletter.com/dermatology/platelet-rich-plasma-prp/
- Sánchez M, Anitua E, Delgado D, et al. Platelet-rich plasma, a source of autologous growth factors and biomimetic scaffold for peripheral nerve regeneration. Expert Opinion on Biological Therapy. 2017;17(2):197-212. doi:10.1080/14712598.2017.1259409


Leave a Reply